Introduction
Aleukemic Leukemia cutis (ALC) is the primary extramedullary cutaneous infiltration of neoplastic leukemic cells that occasionally precede systemic leukemia diagnosis. This study aimed to investigate the clinical characteristics, management, and outcomes of ALC patients to expand our knowledge of this rare entity.
Patients and methods
PubMed, ScienceDirect, Scopus, Web of Science, CINAHL, SpringerLink, and Google Scholar academic databases search for "Aleukemic Leukemia Cutis" case reports between 2000 and 2020.
Results
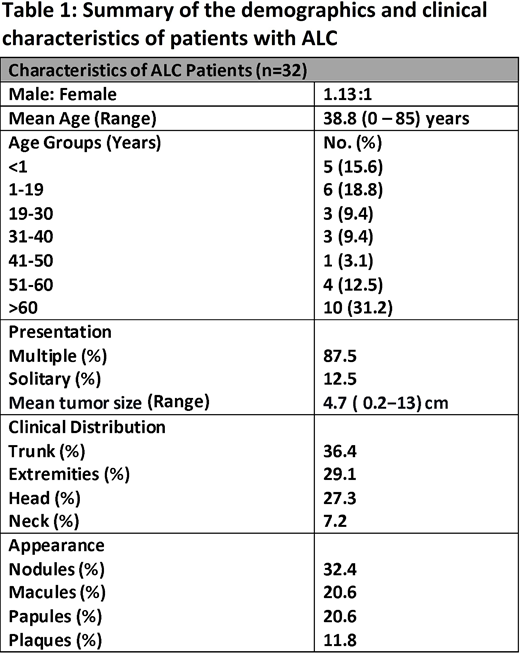
The mean age at the time of diagnosis of the 32 histologically-proven ALC cases included in the study was 38.8 (range, 0-85) years with a male: female ratio of 1.13:1. Regarding the age groups, we recorded 5 (15.6%), 6 (18.8%), 3 (9.4%), 3 (9.4%), 1 (3.1%), 4 (12.5%), and 10 (31.2%) patients in the age groups of <1, 1-19, 19-30, 31-40, 41-50, 51-60, >60 years, respectively. The mean interval between ALC presentation and leukemia-diagnosis was 9.7 (range, 0-48) months, including a patient with a 20-months interval who underwent chemotherapy and cord-blood stem cell transplantation (SCT) later found to have acute myeloblastic leukemia (AML) relapse at 84-months from the initial ALC diagnosis.
Lesions were multiple in 87.5% and solitary in 12.5% of cases, located most commonly, in decreasing order, in the trunk, extremities, head, and neck in 36.4%, 29.1%, 27.3%, and 7.2 % of cases, respectively. Nodules, macules, papules, and plaques were the four most common lesions in 32.4%, 20.6%, 20.6%, and 11.8% of cases, respectively, whereas swelling, patches, and ulcers were uncommon. Lesions were described as erythematous and violaceous in 35.3%, and 2.9% of cases, respectively, with mean tumor dimensions of 4.7 (range, 0.2−13) cm. Following ALC diagnosis, a clinically identifiable systemic disease was detected in 12/32 (37.5%) cases, out of which AML was the most common type, found in 7 (58.3%) cases, followed by precursor B-cell acute lymphoblastic leukemia (preB ALL) in 2 (16.6%) case. Less common types were myelodysplastic syndromes (MDS), acute promyelocytic leukemia (APL), and biphenotypic acute leukemia (BAL) constituted 3 (25.0%) cases collectively.
Among 25 patients with available data on treatment modalities, the most common overall was chemotherapy in 22 (88.0%) cases, out of which 13 (59.1%) had chemotherapy alone, 6 (27.3%) had chemotherapy plus SCT, and 3 (13.6%) cases had chemotherapy plus either radiotherapy, surgery plus chemoradiation or electron beam therapy. The mean duration of follow-up was 16.6 months (range, seven days-100 months). Furthermore, of the 27 patients with reported data, 12 (44.4%) were alive upon follow-up, out of which 7 (58.3%) disease-free, 4 (33.3%) in remission, and 1 (8.3%) with persistent disease, and fifteen (55.6%) patients died of the disease.
Discussion
Our study's main findings are as follows: First, 14 (43.7%) patients were older than 50 years of age, with an incidence only slightly higher in males than females. Second, lesions were mostly multiple and may take various forms of presentation, with nodules being the most common finding in over one-third of cases. Third, concurrent diagnosis of systemic disease was reported in 37.5% of cases with AML constituting 58.3% of cases. Fourth, chemotherapy was the mainstay of the treatment, followed by SCT in almost one-third of the cases. Notably, more than half of the patients died within months after ALC diagnosis.
Conclusion
ALC pathology remains not well delineated, and despite all assorted interventions; still, most patients succumb within months of diagnosis. Increased awareness among primary care physicians and dermatologists, amalgamated with further research to further investigate its pathology and determine extramedullary molecular targets, could eventually improve outcomes of this rare but life-threatening ailment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal